Other vertical hyperechoic artefacts may mimic the B-line, but these artefacts always become less hyperechoic or completely fades out.
In comparison, B-lines never fade out and can be visualised the entire way to the bottom of the field of view.

Other vertical hyperechoic artefacts may mimic the B-line, but these artefacts always become less hyperechoic or completely fades out.
In comparison, B-lines never fade out and can be visualised the entire way to the bottom of the field of view.

The presence of a characteristic artefact known as a B-line can be used as an indirect marker of lung disease.
B-line artefacts occur when the density of the lung has increased as for example in interstitial oedema or pulmonary fibrosis.
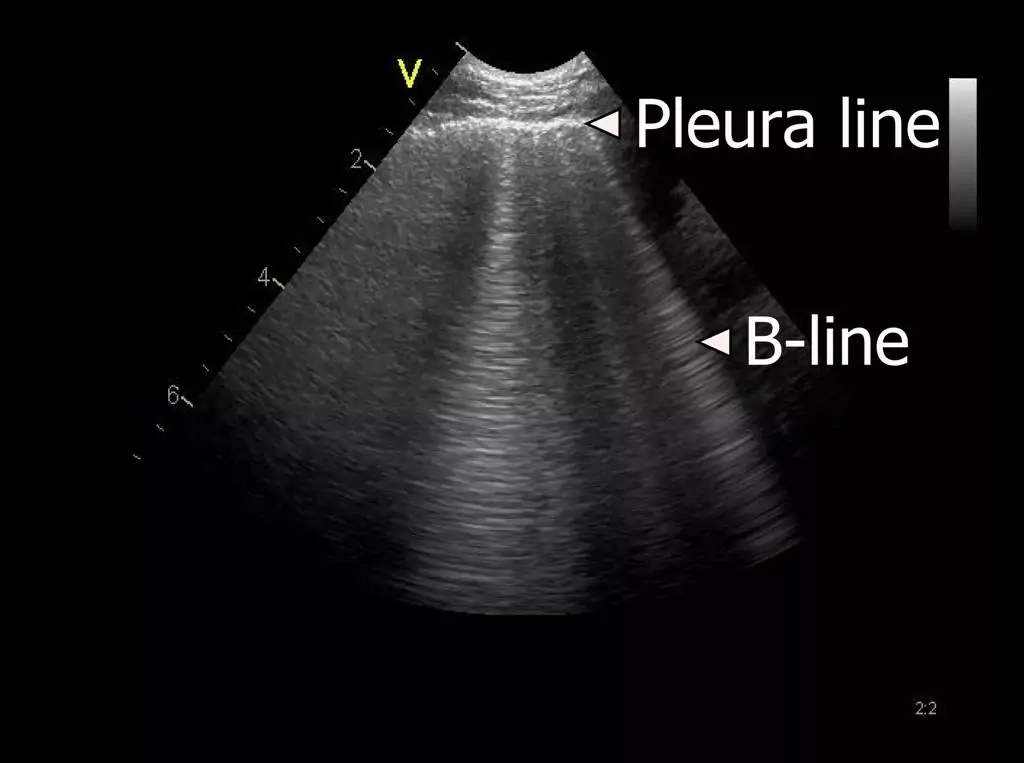
This lesson describes the B-line artifact and the interstitial syndrome (IS) in more detail.

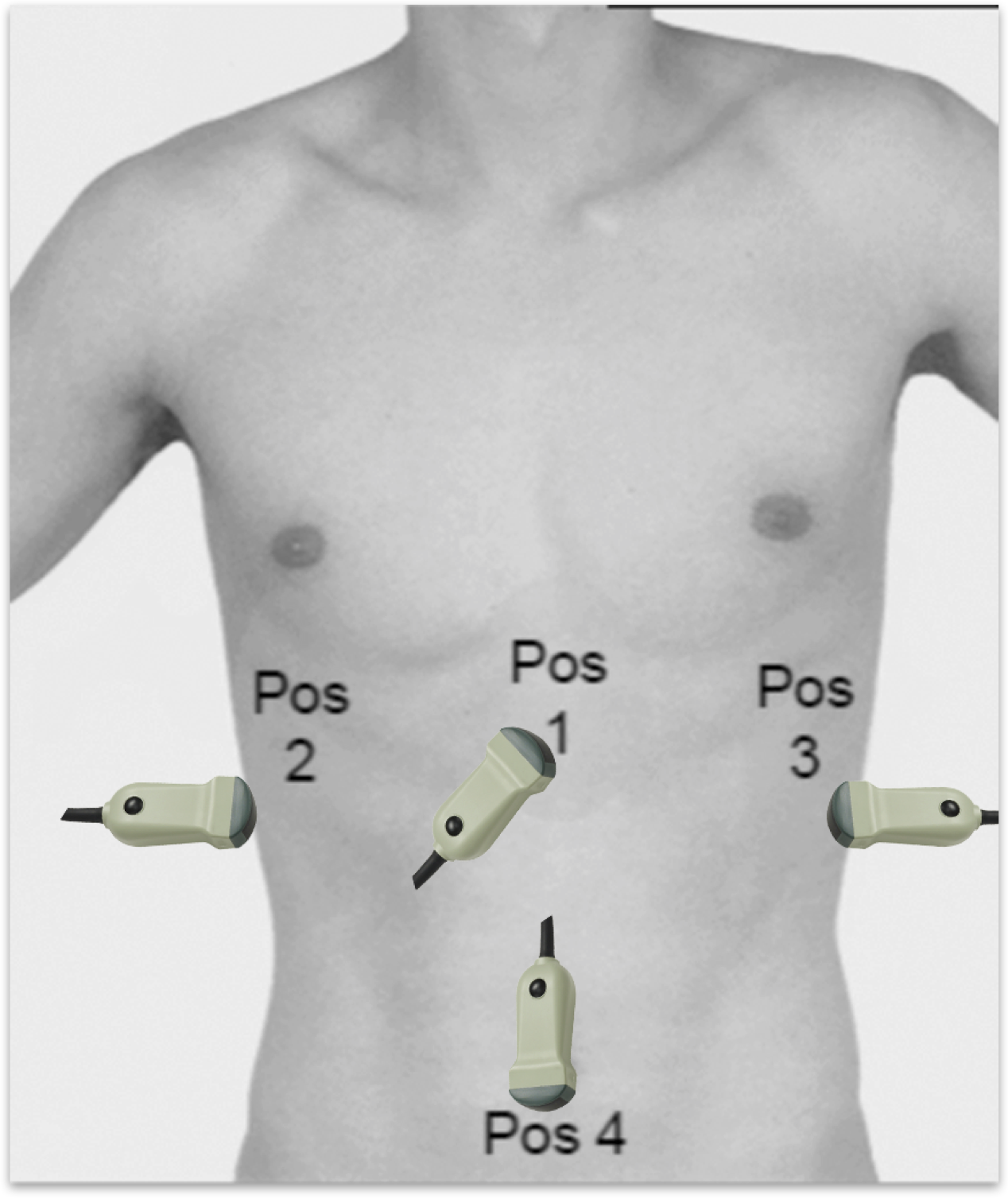
When performing FLUS, each hemithorax can be divided into an anterior, lateral and posterior surface, which can be further subdivided into smaller squares, representing a scanning zone, which should be assessed using FLUS*.
Each of the scanning zones can be denoted from 1R to 7R (R = right) and 1L to 7L (L = left).

In order to save time, the two lateral transducer positions used for the evaluation of possible pleural effusion can easily be integrated with the transducer placement used for the evaluation of the hepatorenal fossa and splenorenal fossa normally performed as a part of a FAST examination.

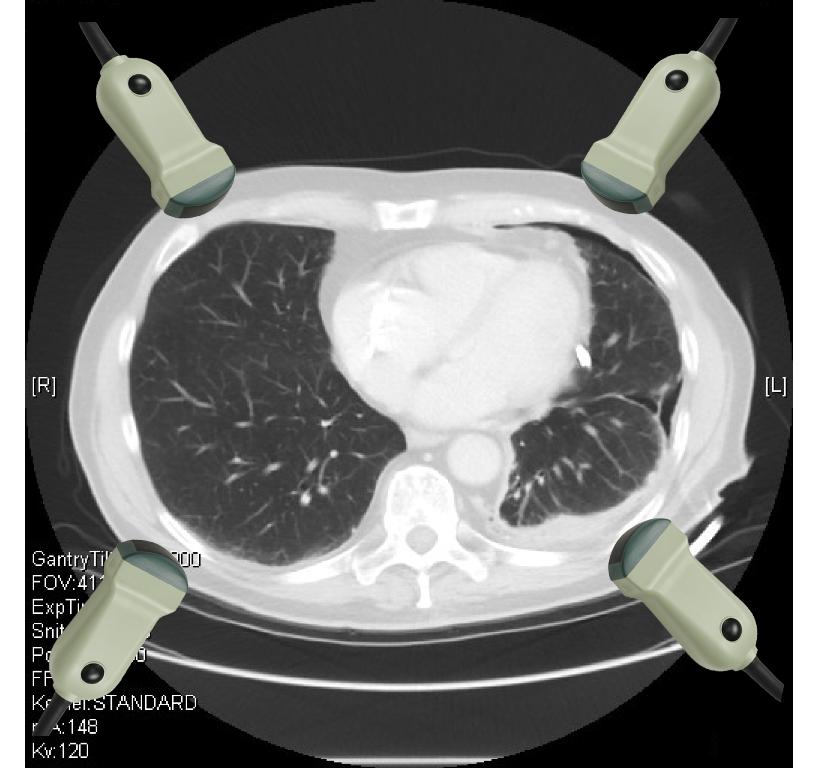
Four positions for transducer placement are used for the thoracic evaluation in E-FAST.
Two anterior positions are used for the evaluation of pneumothorax and two lateral positions are used for the evaluation of pleural effusion.
Anterior positions:
– Right hemithorax: 2. Intercostal space in the medioclavicular line
– Left hemithorax: 2. Intercostal space in the medioclavicular line
Lateral positions:
– Right hemithorax: 4. Intercostal space in the posterior axillary line
– Left hemithorax: 4. Intercostal space in the posterior axillary line

When performing E-FAST it is advantageous to use the low-frequency abdominal transducer for the entire examination.
Supplementary use of a high-frequency transducer can be considered if there is doubt whether lung sliding is present or not.

The FAST protocol is described in detail in a separate USabcd e-course. Only the principles on how to perform FLUS as a part of the FAST examination are described in this lesson.
When performing FLUS as a part of the E-FAST, the purpose is to answer the following two yes or no questions:
– Is a pneumothorax present?
– Is a pleural effusion present?
FAST (Focused Assessment with Sonography for Trauma) is a simple, quick and safe method for the diagnosis of free fluid in the pericardium and peritoneum.
Several studies have demonstrated that FLUS performs better than conventional chest X-rays in the diagnosis of pneumo- and hemothorax in trauma patients.
On this basis, FLUS has been integrated with the FAST protocol into the socalled Extended-FAST (E-FAST) in order to improve diagnosis of pneumo- and hemothorax in the traumatised patient.
As with other types of ultrasound examinations, correct placement of the orientation marker (OM) on the transducer is essential in order to ensure correct orientation of the ultrasound image on the screen and corresponds to the orientation of the structure scanned.
Most often FLUS is performed with the transducer placed in the vertical plane above an intercostal space.
When scanning in the vertical plane the OM should be facing cranially.
If supplementary scanning in the transversal plane is performed, the transducer should be rotated counterclockwise so the OM faces the patient’s right side.
