Despite the recent publication of international consensus guidelines* concerning the use of FLUS, there is no international consensus on how to perform FLUS.
In this lesson, two approaches are described:
– LUS as a part of the E-FAST
– FLUS
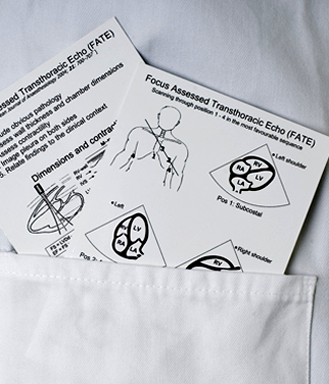
LUS is also performed as a part of other focused ultrasound protocols (e.g. FATE, RUSH) – the approaches used in these protocols are not described in this lesson.
* Volpicelli, G., et al., International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med, 2012. 38(4): p. 577-91.