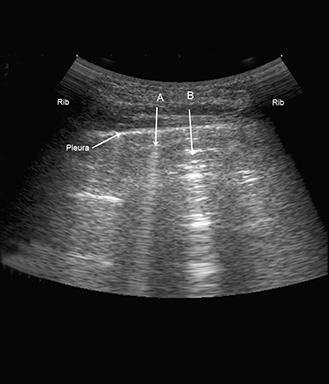
Once the anterior and lateral surfaces have been scanned, the patient is asked to sit up and the squares on the posterior surface are scanned using the same principles as described for the anterior and lateral surfaces
Again in each scanning zone it is noted whether pneumothorax, pleural effusion or multiple B-lines are present or whether only normal findings are present