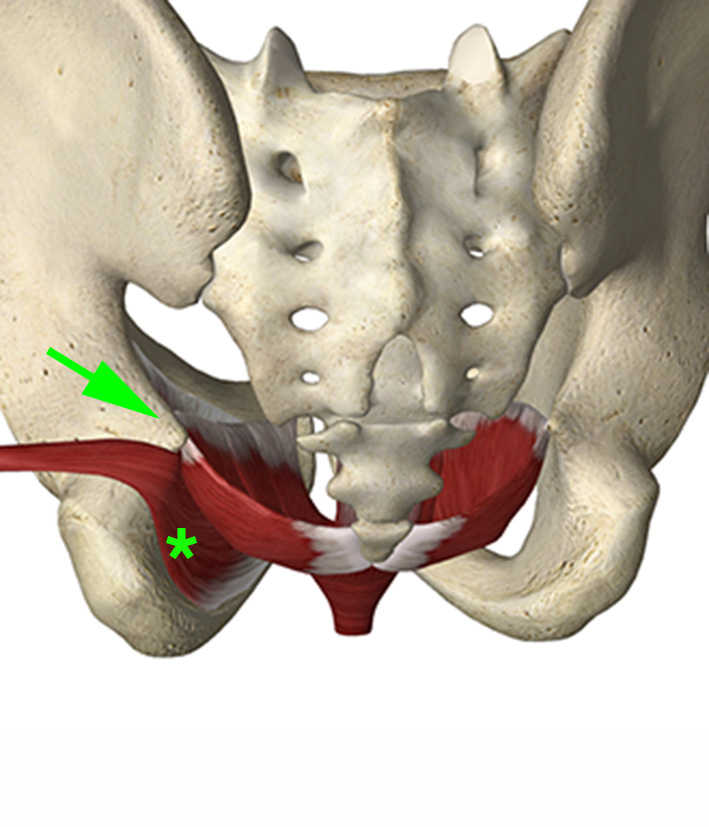
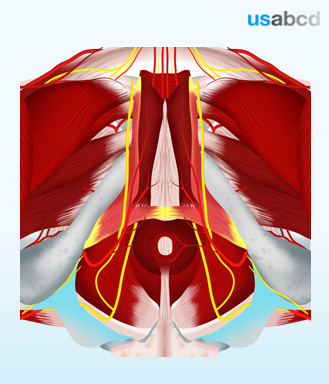
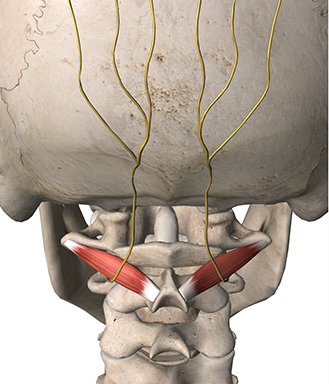
The deep pelvic floor consists of the levator ani muscles which has two major components: The pubovisceral and the iliocyccygeal muscles.
The two pubovisceral muscles are the pubococcygeus and the puborectalis muscles.
The puborectalis muscle origins from the posterior surface of the pubic bone and inserts around the rectum. It supports the contraction of the anal sphincter.
The pubocyccygeus muscle origins from the posterior surface of the superior pubic ramus and inserts on the coccyx.
The iliococcygeal muscle origins from the ischial spine and the obturator internal muscle fascia.
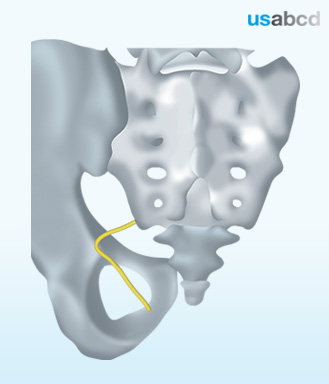
The levator ani muscles are all innervated by direct branches of the ventral primary rami of the spinal nerves S2-S4.