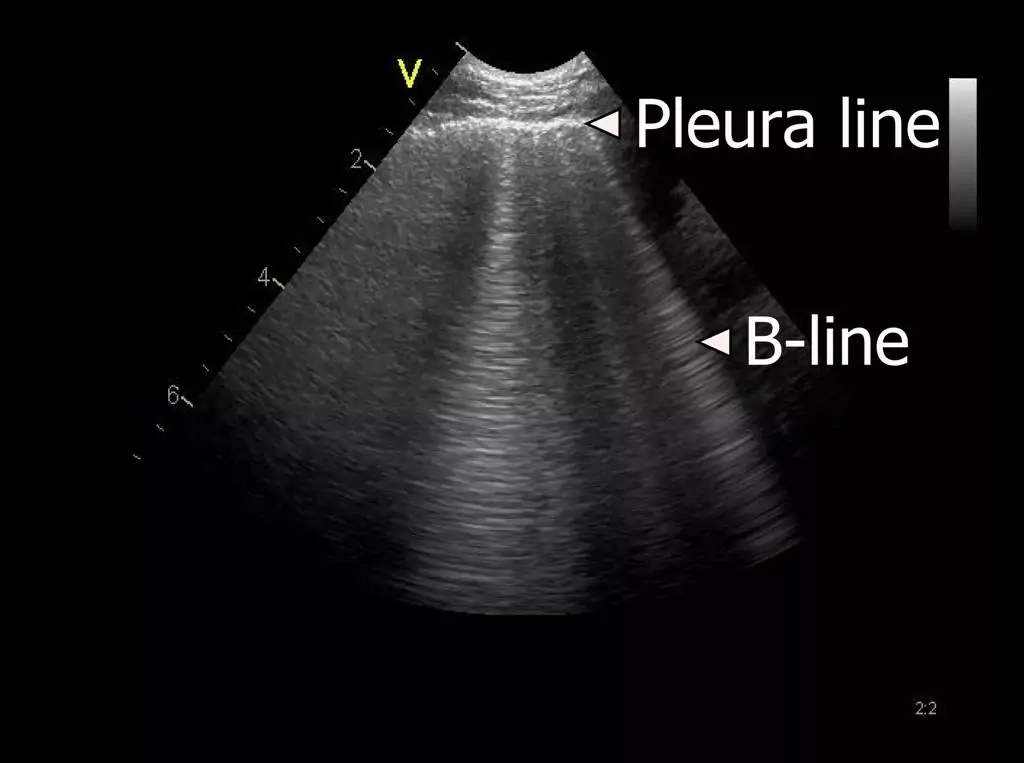
As an example of a setting where focal B-lines still can be clinical useful, would be in a patient with clinical suspicion of pneumonia.
A lobar pneumonia with resulting increased density of the lobe, with corresponding B-lines would confirm the clinical suspicion.
If the density further increases and the lung tissue is filled with fluid and secretions the pattern will change to that of lung consolidation.