Based on patient history and primary assessment, a list of some of the most common and important differential diagnoses would be:
– COPD exacerbation
– Heart failure with pulmonary edema
– Pneumonia
– Pulmonary embolism
– Pleural effusion
– Pneumothorax
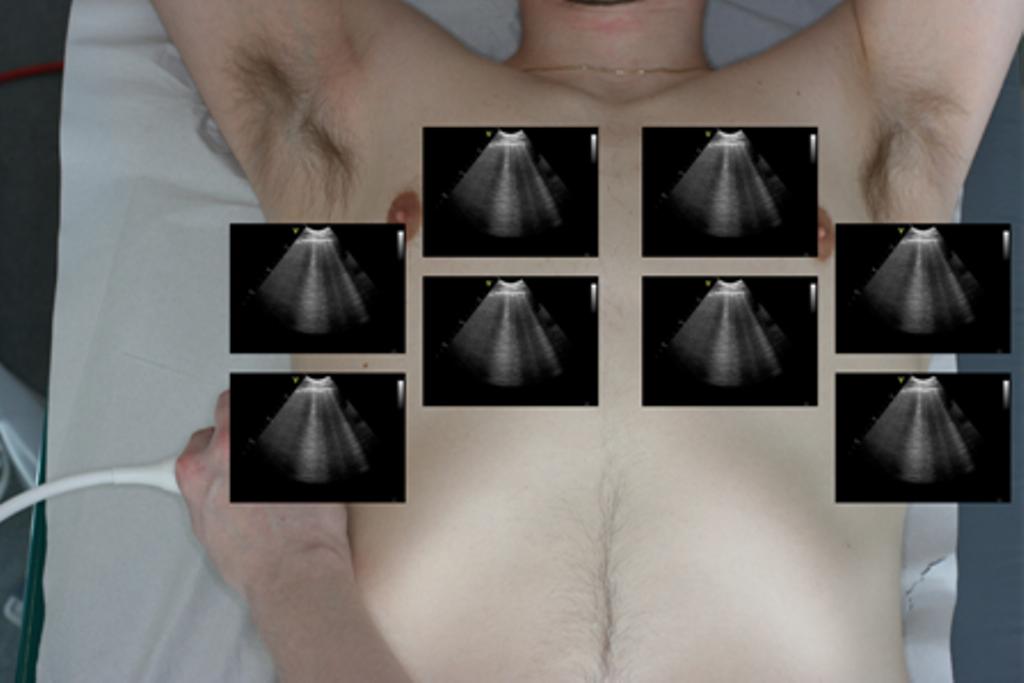
FLUS high feasibility and diagnostic capabilities warrants its use as a standard diagnostic test in patients with respiratory symptoms