A pneumothorax is ruled out
• When lung sliding/pulse or B-lines can be seen on the anterior part of the thorax (in a patient lying on the back)
A pneumothorax is suspected
• When neither lung sliding/pulse nor B-lines can be seen on the anterior part of the thorax
A reliable diagnosis of pneumothorax can be established
• When neither lung sliding/pulse nor B-lines can be seen on the anterior part of the thorax AND
• A lung point is detected
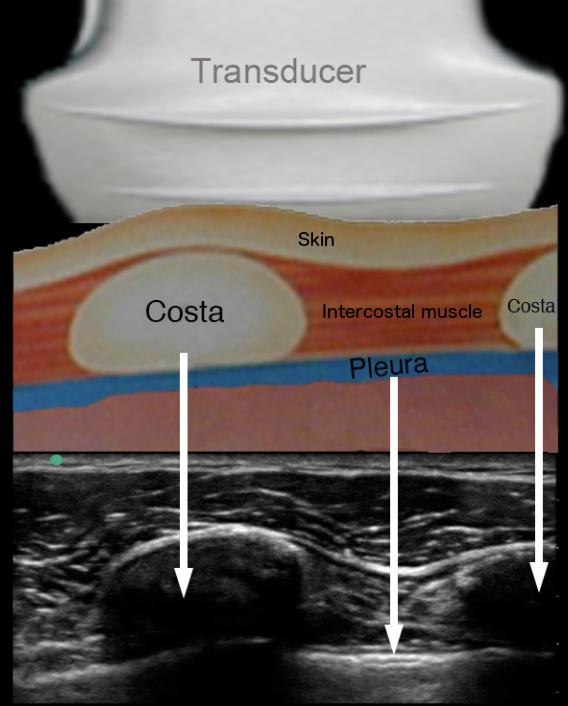
Ok, so lung sliding, some weird lines and a lung point – how do I do this in real life?
– Look at the video on the next page
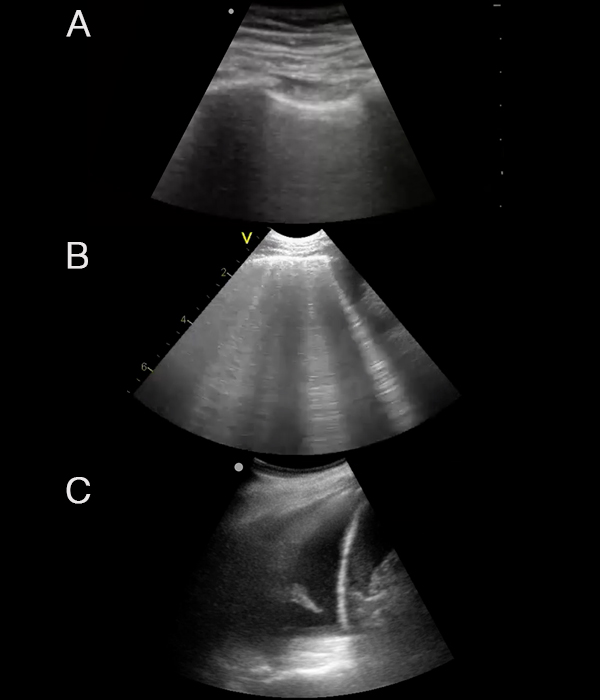
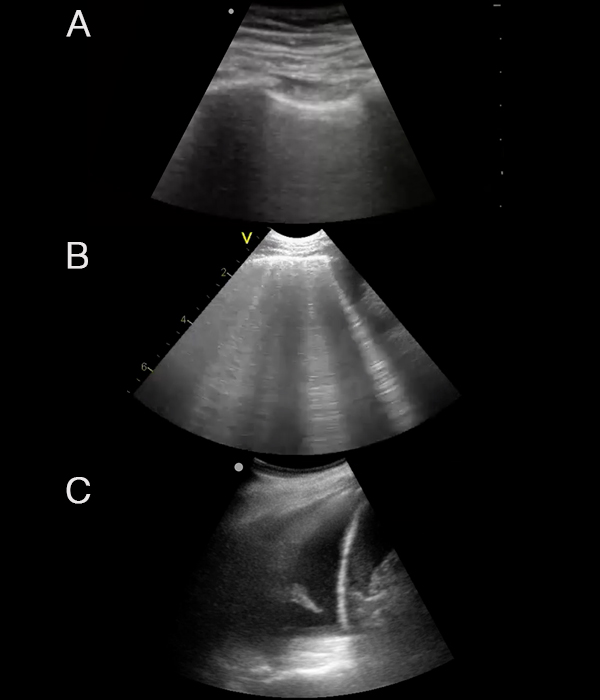
B: No lung sliding – PTX is possible