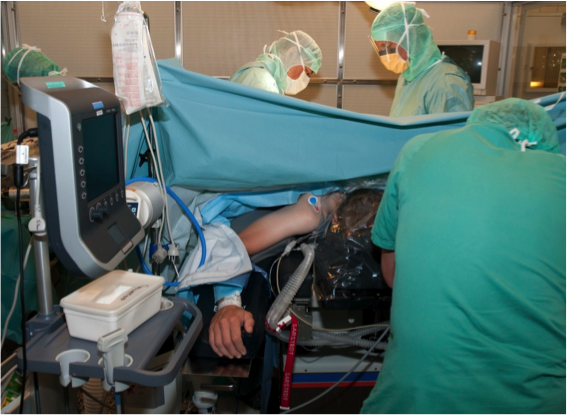
Since FLUS is used in critically ill patients in a variety of settings (e.g. prehospital, ED, ICU, OR) it may not always be possible to perform a standardised FLUS examination.
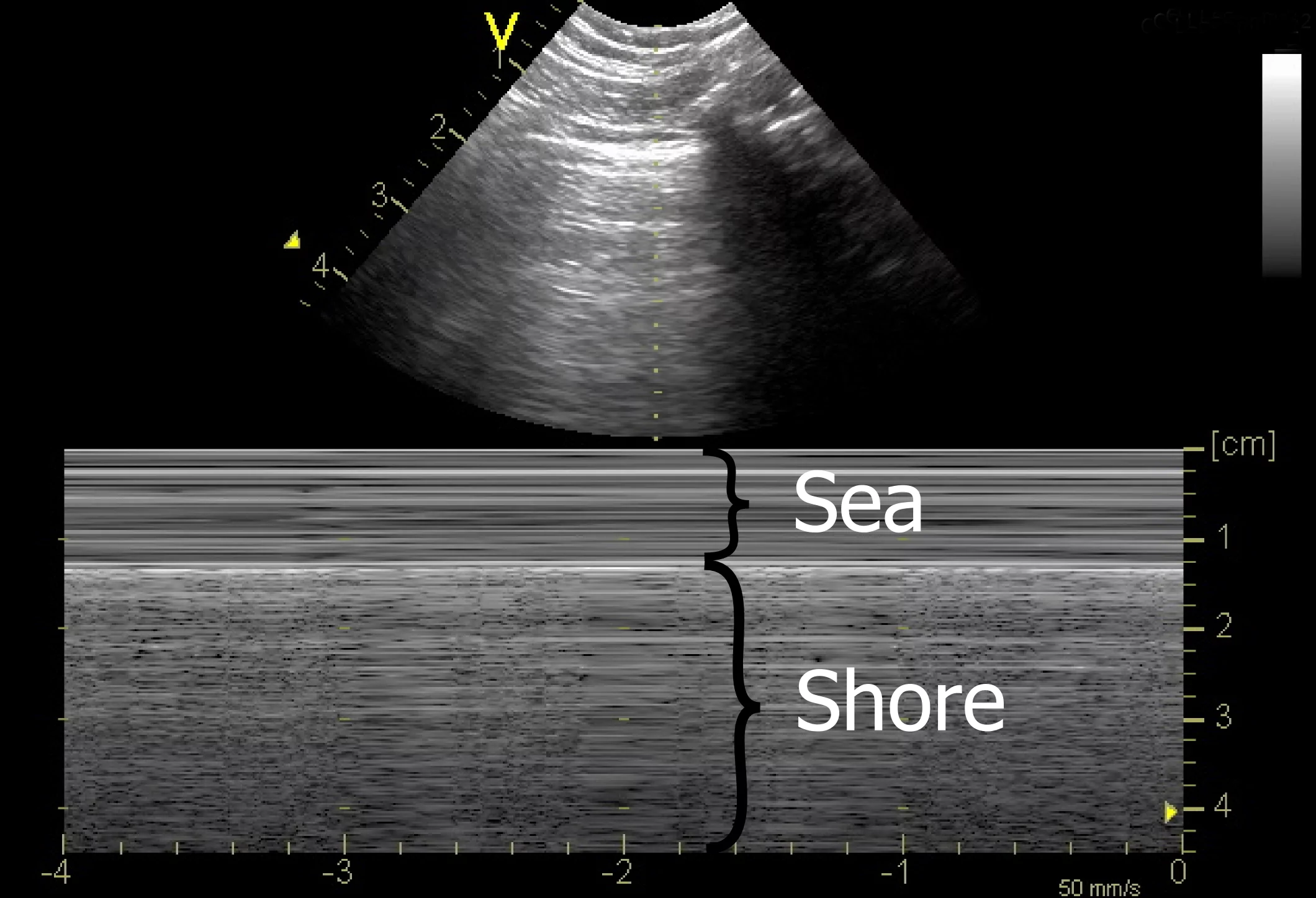
By using FLUS in a standardised and systematic approach, however, the examination still has a very high feasibility and the diagnosis and exclusion of important diagnoses such as pneumothorax, pleural effusion and interstitial syndrome can often still be made.