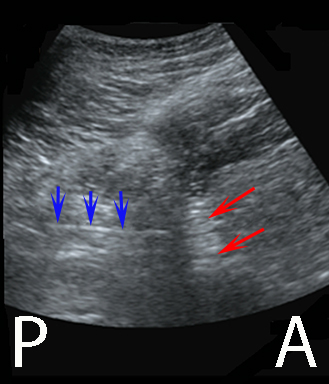
In the starting position of the probe the characteristic continuous, hyperechoic iliac bone is visualized
In the starting position of the probe the characteristic continuous, hyperechoic iliac bone is visualized
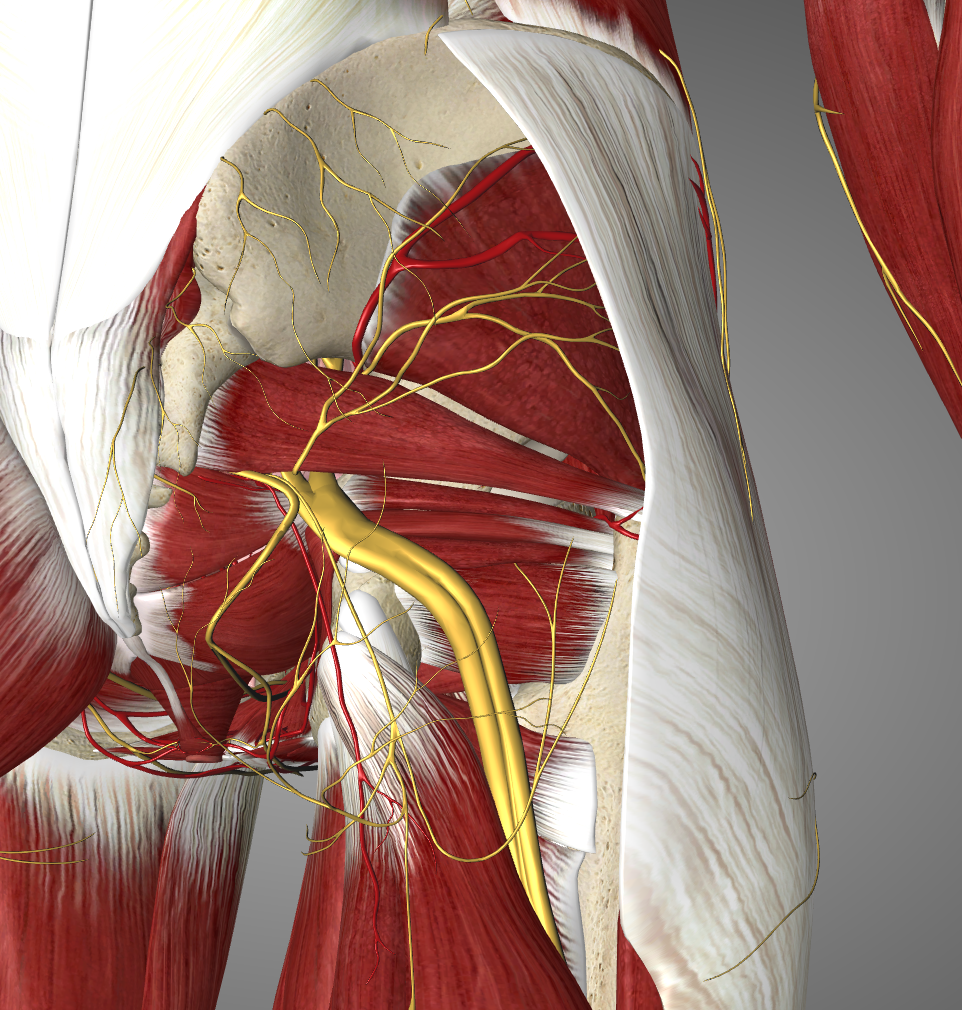
The needle penetrates the gluteus maximus and the piriformis in order to reach the target sacral plexus in the greater sciatic foramen between the sacral bone and the ischial bone
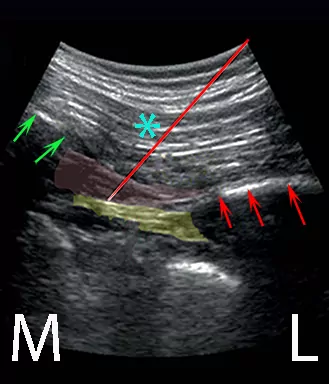
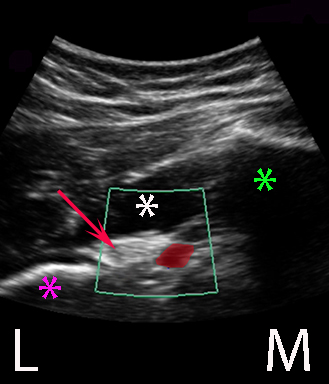
It is important to visualize the inferior gluteal artery medially next to the sacral margin
It indicates the correct level of needle insertion and it is a safeguard that allows you to avoid piercing the artery during needle insertion
Bendtsen TF, Lönqvist PA, Jepsen KV, Petersen M, Børglum J: Preliminary results of a new ultrasound-guided approach to block the sacral plexus: The parasacral parallel shift. Br J Anaesth 107(2): 278-80 (2011)
Removal of the gluteus maximus muscle reveals the emergence of the sciatic nerve from the sacral plexus at the lower border of the piriformis muscle
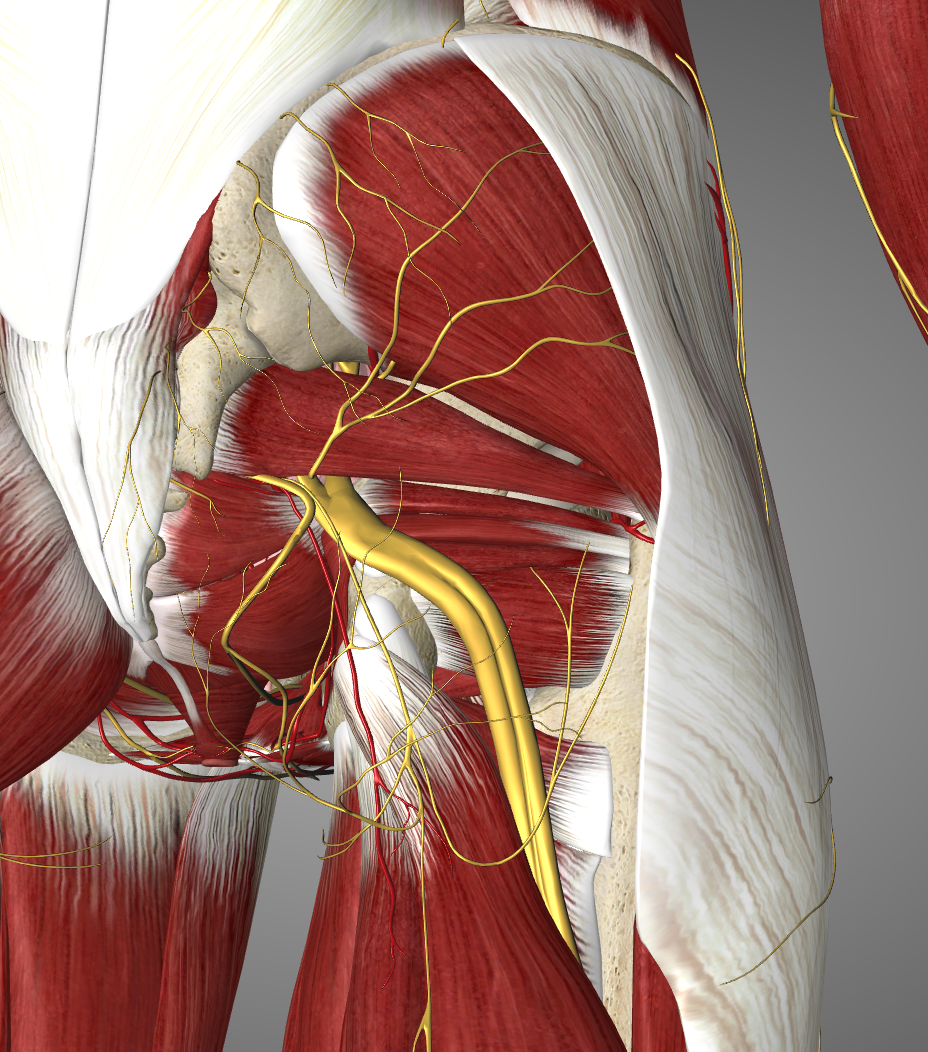
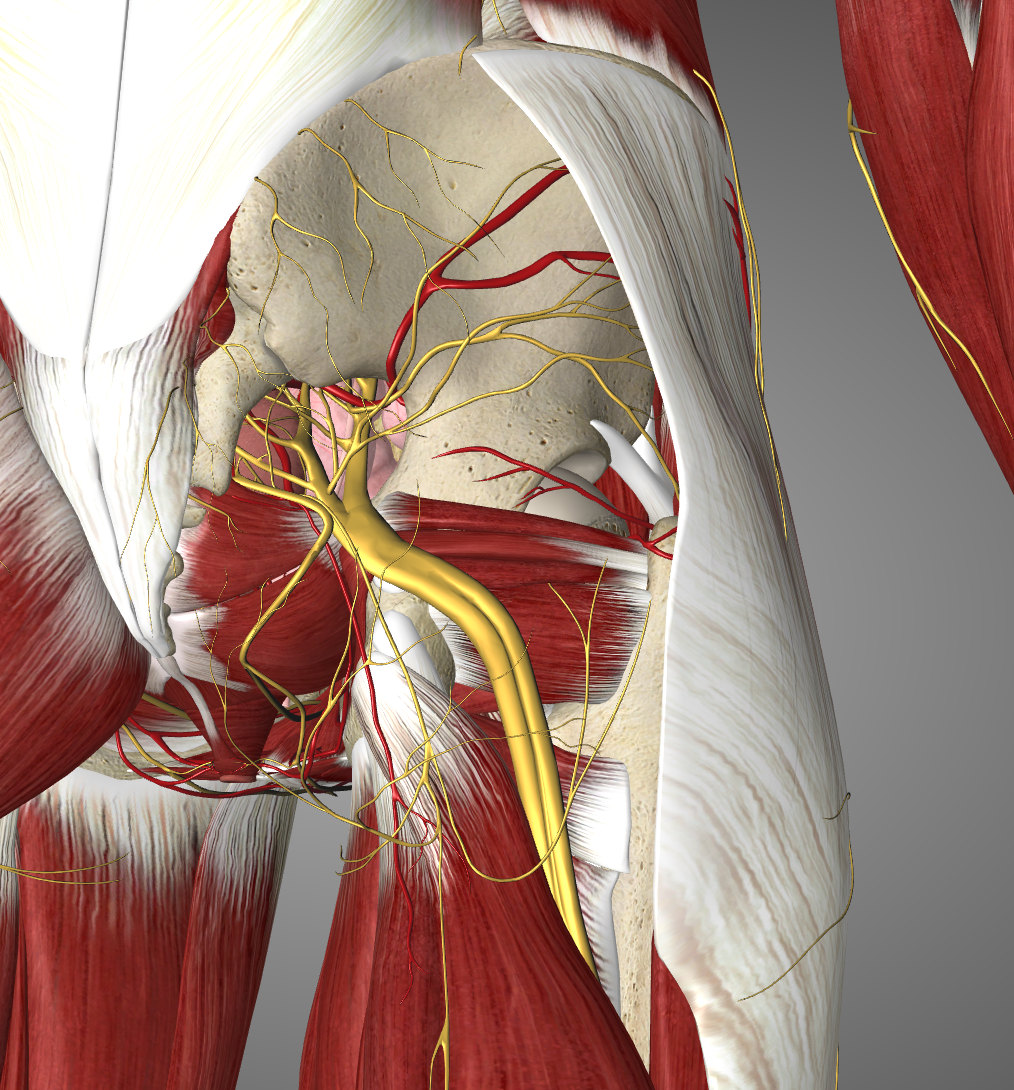
Removal of the gluteus medius muscle reveals the iliac bone that is an important marker of the parasacral parallel shift technique
After removal of the gluteus minimus muscle, the major part of the iliac bone is exposed
The superior gluteal artery runs across the iliac bone
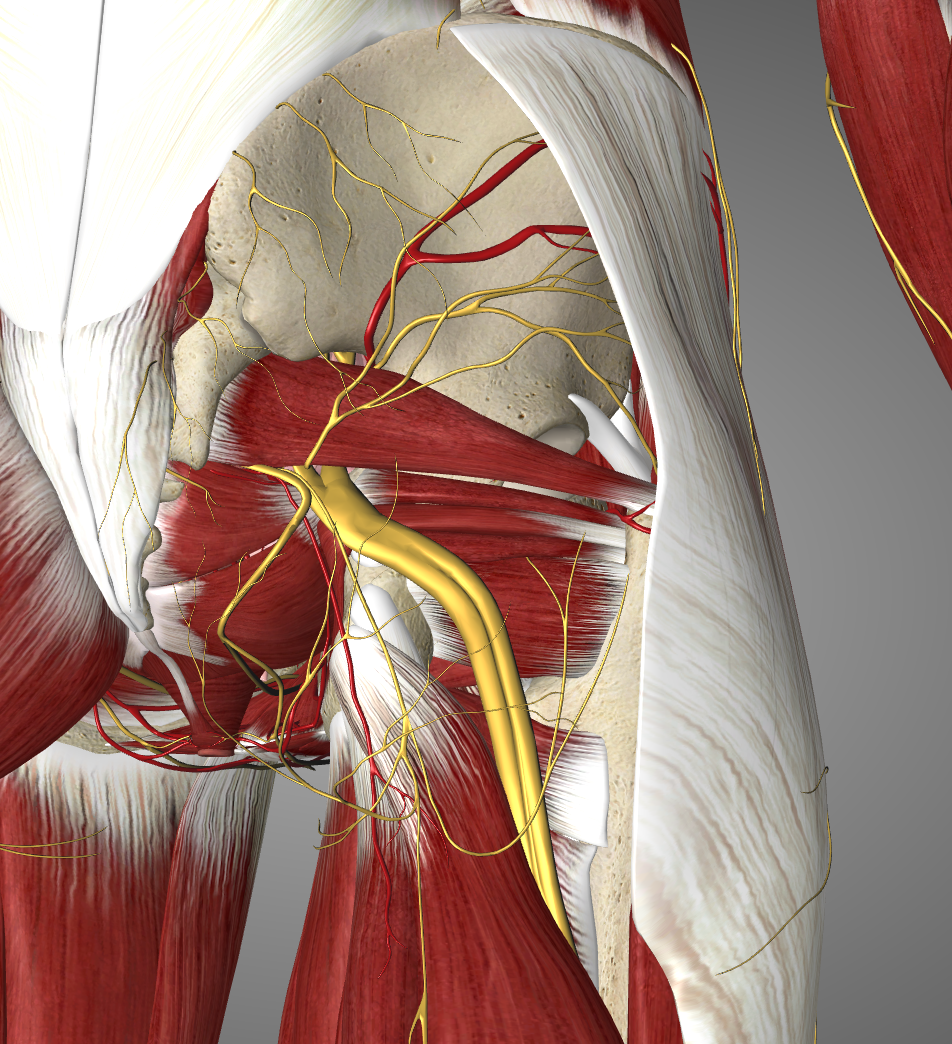
Removal of the piriformis muscle reveals the sacral plexus as it emerges from the greater sciatic foramen
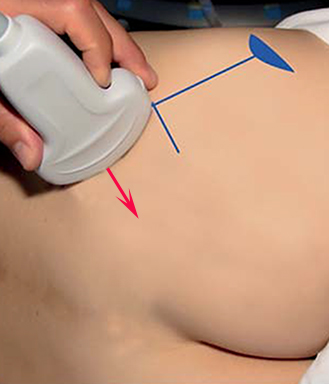
The curved array probe is placed on the upper half of the line connecting the posterior superior iliac spine and the ischial tuberosity; in this position the iliac bone line is a continuous hyperechoic line (see next page)
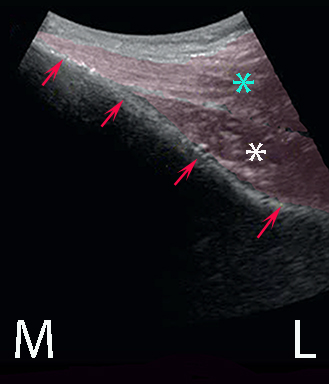
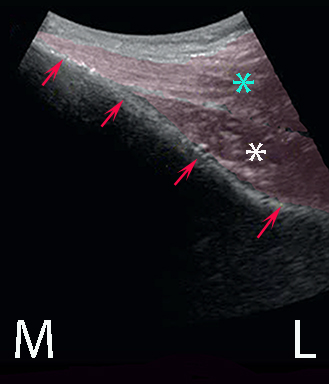
From this starting position the probe is parallel shifted infero-medially until the continuity of the iliac bone is disrupted. It is disrupted because the probe reaches the pelvic opening where the sacral plexus exits the pelvis – the greater sciatic foramen (see second next page)
With a slight caudal tilt of the probe, the sacral plexus becomes visible underneath the piriformis muscle (see second next page)
The needle is inserted from the lateral end of the probe and the needle tip is advanced until it reaches the target lumbar plexus (see second next page); electrical nerve stimulation can be used to confirm the endpoint
10-15 mL of local anaesthetic is injected in the fascial space between the piriformis muscle and the strong pelvic fascia
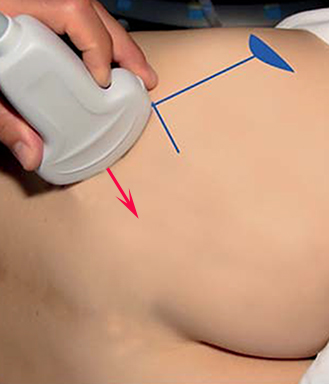
The needle is inserted from the back of the patient practically parallel to the foot print of the probe
This makes it easy to visualize the needle with ultrasound