After having completed the e-learning module, the next step is to attend one of our hands-on-training (HOT) courses
You can join any one of these which are offered in more than 20 different countries
All aAdvanced FATE courses are standardised with a comprehensive and very structured learning program
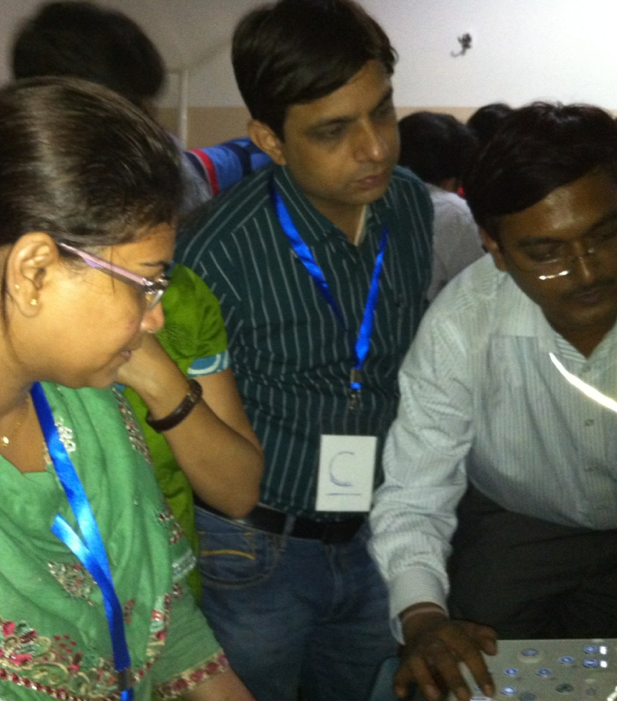
The courses are lead by one of our experienced chief instructors who ensures that all learning objectives are fulfilled while the supervisors at the workstations are often local experts
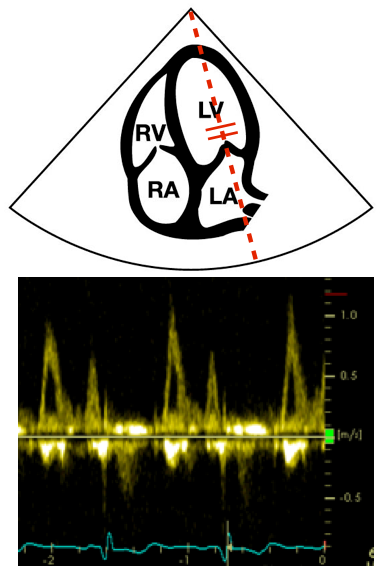
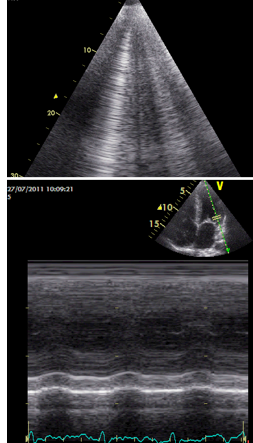
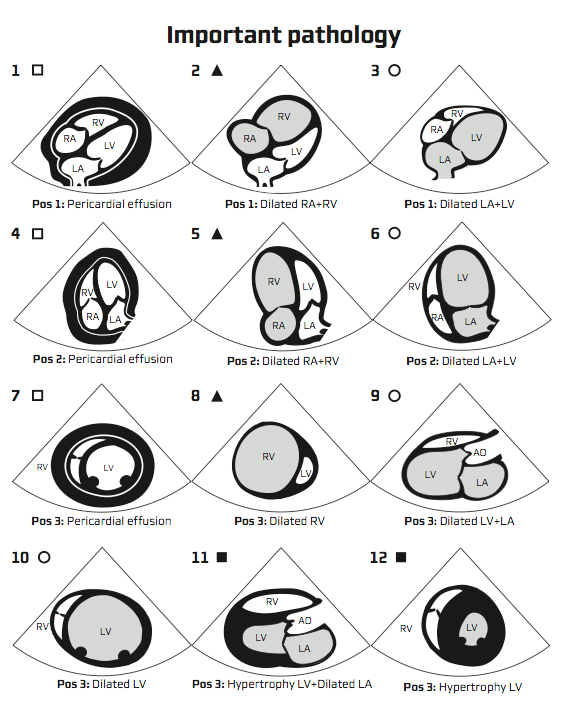
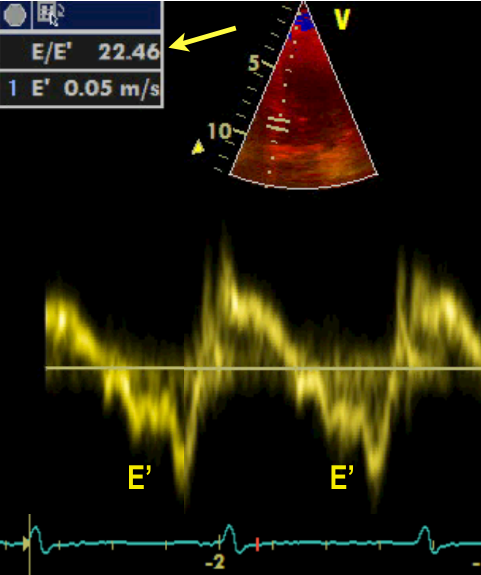
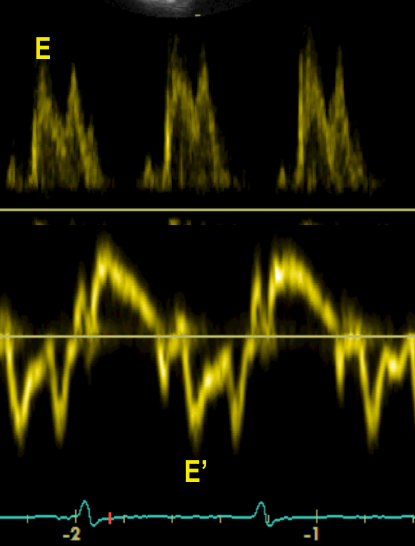
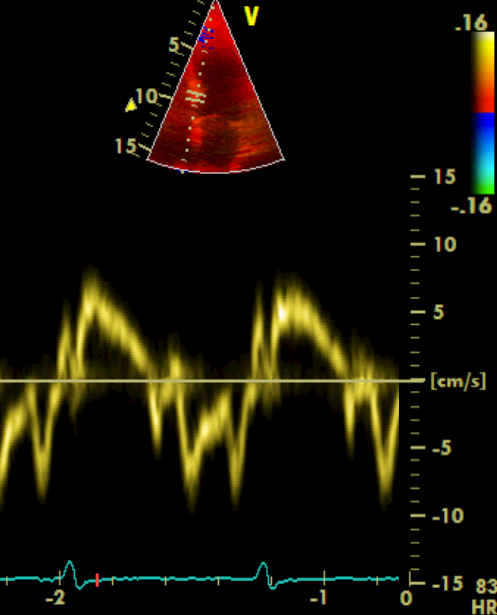
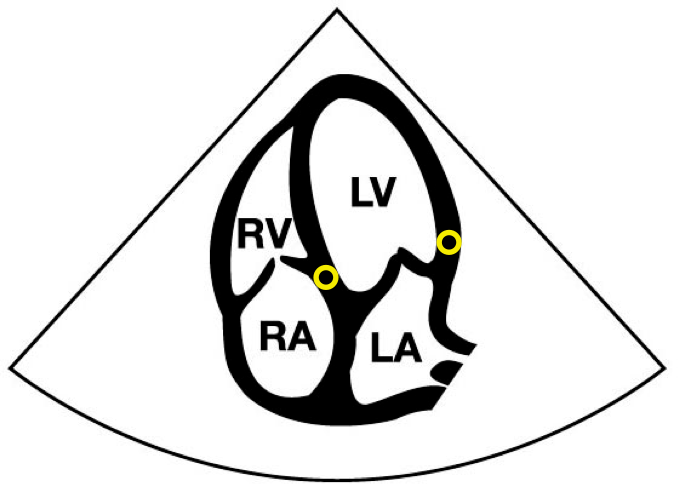
After the Advanced FATE course you will be able to use 2D, pulsed wave and tissue Doppler imaging for the evaluation of diastolic function
If you want to see the content of HOT 3 click on “Read more”